My patient is a 6.5-year old male neutered Belgian Malinois who has a history of weight loss and intermittent vomiting of 3-weeks duration.
A CBC and serum chemistry panel were both unremarkable, with normal serum sodium and potassium values. Abdominal ultrasonography was performed, which revealed a splenic mass. A splenectomy and liver biopsy were performed, which revealed a splenic hematoma and hepatopathy, thought to be secondary to Rimadyl (1). The drug has subsequently been discontinued with no improvement.
Today we did an ACTH stimulation test to rule out Addison's disease, using a dose of 2.2 U ACTH gel administered intramuscularly. The baseline cortisol value was 2.2 μg/dl (reference range, 1-4 μg/dl) and the 2-hour post-ACTH cortisol was 3.6 μg/dl (reference range, 6-20 μg/dl).
Is this subnormal cortisol response consistent with mild Addison's disease?
My Response:
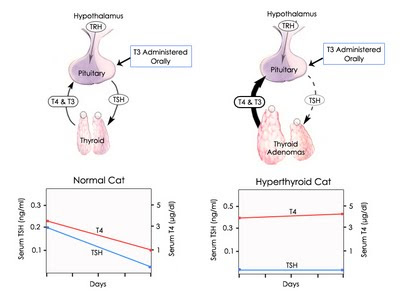
This ACTH stimulation test completely rules out spontaneous hypoadrenocorticism (Addison's disease). Most dogs with primary, secondary, or atypical hypoadrenocorticism will have a low basal cortisol concentration (< 1 μg/dl) and all will have a baseline cortisol value that is less than 2 μg/dl (2-4).
After ACTH stimulation, dogs with hypoadrenocorticism tend not to have any cortisol response to ACTH stimulation, and post-ACTH cortisol values should never be greater than 2.5-3.0 μg/dl (see Figure below)
In many dogs, the blunted cortisol response, as seen in this dog, is either due to prior administration of glucocorticoid sometime in the last few weeks. However, in this dog, the likely cause for the subnormal cortisol response is the compounded ACTH preparation that you used.
In a study performed a few years ago (5), normal dogs were tested with cosyntropin (Cortrosyn, 5 μg/kg, IV) and 4 different compounded forms of ACTH (all manufacturers recommend a dose of 2.2 U/kg, IM). For all 5 of the ACTH stimulation tests, samples for cortisol analysis were collected before and 1 and 2 hours after ACTH injection.
After administration of the 4 forms of compounded ACTH, the time to reach peak cortisol concentrations varied, with some dogs showing the maximal cortisol value at 1 hour and others having peak cortisol concentrations at 2 hours.With 2 of the 4 products, serum cortisol concentration returned to baseline values by 2 hours in many of the dogs.
Thus, due to variability in duration of cortisol response after injection of the compounded ACTH products, the investigators recommend that we need to collect several post-ACTH samples for cortisol analysis after administration of a compounded ACTH preparation to ensure that we detect the peak cortisol response. At the minimum, we recommend collecting samples at 1 and 2 hours following injection.
Because of this variability in cortisol stimulation, I'm not a fan of using compounded ACTH preparations. I would rather use low-dose Cortrosyn (6) and collect only one post-ACTH blood sample at 1-hour and be assured that will produce the maximal cortisol response at that time.
References:
- MacPhail CM, Lappin MR, Meyer DJ, et al. Hepatocellular toxicosis associated with administration of carprofen in 21 dogs. Journal of the American Veterinary Medical Association 1998; 212: 1895-1901.
- Lifton SJ, King LG, Zerbe CA. Glucocorticoid deficient hypoadrenocorticism in dogs: 18 cases (1986-1995). Journal of the American Veterinary Medical Association 1996;15;209:2076-2081.
- Cook AK, Bond KG. Evaluation of the use of baseline cortisol concentration as a monitoring tool for dogs receiving trilostane as a treatment for hyperadrenocorticism. Journal of the American Veterinary Medical Association 2010;237:801-805.
- Klein SC, Peterson ME. Canine hypoadrenocorticism: part II. Canadian Veterinary Journal 2010;51:179-184.
- Kemppainen RJ, Behrend EN, Busch KA. Use of compounded adrenocorticotropic hormone (ACTH) for adrenal function testing in dogs. Journal of the American Animal Hospital Association 2005;41:368-372.
- Martin LG, Behrend EN, Mealey KL, et al. Effect of low doses of cosyntropin on serum cortisol concentrations in clinically normal dogs. Journal of the American Veterinary Medical Association 2007;230:555-560.