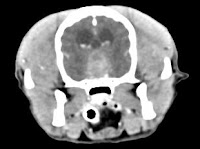
His hyperadrenocorticism has responded well to medical therapy with mitotane. However, over the last few months, the dog developed severe lethargy and inappetence. More recently, he exhibited behavior changes, severe altered mentation, and had a seizure. We did a CT scan (see dog's image above), which confirmed a large pituitary tumor.
I have many questions about this dog:
- Are large, invasive pituitary tumors like this common in dogs with Cushing's disease?
- Can surgery be used to remove the pituitary tumor?
- Or is this case a poor surgical candidate, given the large tumor size and location?
- If I do a hypophysectomy, which approach is better — i.e., the transsphenoidal or ventral paramedian approach?
- Or would external radiation therapy be a better choice in this dog?
More than 90% of dogs with pituitary-dependent hyperadrenocorticism (PDH) have an ACTH-secreting pituitary adenoma as the primary cause of their disease. Approximately 50-60% of these dogs with PDH have a pituitary tumor large enough to be visible on CT or MRI scans at the time of diagnosis (1). With time, these pituitary tumors will increase in size over time as they are being treated medically with mitotane or trilostane. Although these therapies are effective at relieving the clinical signs associated with the disease, neither treatment targets the pituitary tumor. Therefore, over time all dogs with PDH are at risk for continued pituitary tumor development, growth, and invasion. It has been estimated that 10% to 25% of dogs with PDH will eventually develop neurologic signs caused by expansion of their pituitary tumor (2).
No, this is not a good surgical case. Surgery in the right hands (i.e., an experienced neurosurgeon who has done large numbers of hypophysectomies over years with consistent positive results) has been shown to be very effective (3,4). However, this dog's pituitary tumor is just too large and invasive to remove with a transphenoid approach (5). A hypophysectomy would only remove the small portion in the sella, but this dog's problem is the large portion above the sella that's compressing the brain. If you were going to really try to remove this, you would probably need to use a subtemporal skull-base approach. Even if you are an experienced neurosurgeon, I would strongly advise against attempting pituitary surgery in this dog.
External radiation therapy is clearly the treatment of choice here. Pituitary radiotherapy works very well to dramatically reduce the size of the pituitary tumor, especially in dogs with PDH that are not showing neurologic signs (6-10).
The success of radiation therapy in dogs with large pituitary macrotumors that are also exhibiting neurologic signs, as in this case, is more variable. Some of these dogs will not even survive long enough to complete the planned treatment because of progression of neurologic signs. In 1 study, a significant correlation was found between relative tumor size (i.e., size of tumor relative to calvarium size) and severity of neurologic signs and between relative tumor size and remission of neurologic signs after irradiation (8).
Unfortunately, based on the fact that this dog has a huge, invasive pituitary tumor and is also showing advanced neurological signs, the prognosis is guarded to poor. That said, I believe it's worth a try if the owners was to try to manage this pituitary macrotumor.
Even if the external radiotherapy does shrink the pituitary mass and control the neurologic signs, it may not result in adequate control of clinical signs of hyperadrenocorticism and medical management may be needed. This is especially true if the pituitary tumor is very large, as it is in this dog (8-10). After radiotherapy, the size of tumors decrease by 25% or more in most dogs with large pituitary tumor and can be totally destroyed in a some.
There are a variety of external radiation therapy methods to choose from (11), including conventional radiotherapy, intensity modulated radiation therapy (IMRT), steriotactic radiosurgery or stereotactic radiation therapy (eg, Cyberknife, Gamma Knife). Unfortunately is that there are no good published data on the comparative efficacy of these different radiotherapy options. There are real differences in cost and availability for these techniques, and all have their advantages and disadvantages. All of these radiation therapy methods can be effective, but they still rely primarily on good treatment planning and input from the radiation oncologist.
References:
- Melián C, M. Pérez-Alenza, D, Peterson ME: Hyperadrenocorticism in dogs, In: Ettinger SJ, Feldman EC (eds): Textbook of Veterinary Internal Medicine: Diseases of the Dog and Cat (Seventh Edition). Philadelphia, Elsevier, 2011, pp 1816-1840.
- Ihle SL. Pituitary corticotroph macrotumors. Diagnosis and treatment. Vet Clin North Am Small Anim Pract 1997;27:287-297.
- Hanson JM, van 't HM, Voorhout G, et al. Efficacy of transsphenoidal hypophysectomy in treatment of dogs with pituitary-dependent hyperadrenocorticism. J Vet Intern Med 2005;19:687-694
- Hara Y, Teshima T, Taoda T, et al. Efficacy of transsphenoidal surgery on endocrinological status and serum chemistry parameters in dogs with Cushing's disease. The Journal of Veterinary Medical Science 2010;72:397-404.
- Hanson JM, Teske E, Voorhout G, et al. Prognostic factors for outcome after transsphenoidal hypophysectomy in dogs with pituitary-dependent hyperadrenocorticism. J Neurosurg 2007;107:830-840
- de Fornel P, Delisle F, Devauchelle P, et al. Effects of radiotherapy on pituitary corticotroph macrotumors in dogs: a retrospective study of 12 cases. Can Vet J 2007;48:481-486.
- Goossens MM, Feldman EC, Theon AP, et al. Efficacy of cobalt 60 radiotherapy in dogs with pituitary-dependent hyperadrenocorticism. J Am Vet Med Assoc 1998;212:374-376.
- Kent MS, Bommarito D, Feldman E, et al. Survival, neurologic response, and prognostic factors in dogs with pituitary masses treated with radiation therapy and untreated dogs. J Vet Intern Med 2007;21:1027-1033.
- Mauldin GN, Burk RL. The use of diagnostic computerized tomography and radiation therapy in canine and feline hyperadrenocorticism. Probl Vet Med 1990;2:557-564.
- Theon AP, Feldman EC. Megavoltage irradiation of pituitary macrotumors in dogs with neurologic signs. J Am Vet Med Assoc 1998;213:225-231.
- LaRue SM. SRS, IMRT, IGRT & other novel radiation technologies now being used in veterinary medicine. Proceeding of the ACVIM Forum, 2010.

My Boston Terrier, age 8 has just been diagnosed with a 13 mm macroadenoma. She is not taking any medications for Cushings. She was dx last week after neck surgery. Her neck was still hurting so the surgeon did a CT. My questions are general. Do dogs take Cushings medication with Radiation? Is radiation ever successful with large tumors? My dog is showing very mild neuro changes. I just thought she was aging. Distant staring, takes awhile to climb stairs, not very active. How do most dogs pass? Related to side effects of medications & liver issues or the brain tumor becoming too large? I just want a general idea of what to look out for if we don't begin medication. Just your past experience. Thank you, Pixie's Mom, Wendy
ReplyDeleteWithout seeing your dog and reveiwing the images, I can't really answer your questions. Most dogs respond at least partially to radiation therapy. But that takes a few weeks to months to have any effect so we use medication (either trilostane or mitotane) to control signs (increased thirst and urination, etc), if needed.
ReplyDeleteOverall, if neurologic signs are present, the prognosis with pituitary macrotumors is guarded to poor. I'd talk to your veterinarian and see a neurologist and radiation oncologist for more information about how to treat your dog and the long-term prognosis.
Hi Dr Peterson,
ReplyDeleteMy 5 year old male Whippet just completed 20 IMRT 10 weeks ago for a pituitary tumor. He was also diagnosed with DI, and Hypothyroidism (borderline to true). Since weaning him off Prednisone he has somewhat remained having PU/PD, and has pretty profound inappetence. He is taking Desmopressin BID and Soloxine BID. We also just added an appetite stimulant & Prilosec (in case of nausea). Could the inappetence be due to the Hypothalamus or hunger part of the brain being affected by the tumor or the radiation? He had body shivers or tremors also during the weeks of IMRT and while still on the Pred, but those have subsided and he is otherwise active, and has no other illness symptoms. Should we increase Desmopressin dose? He is 42lbs. and receives 0.1mg BID. Any thoughts or advice is greatly appreciated. He is a great dog. Thank you in advance.
Unfortunately, I don't have any answers here. The PU/PD could be due to undertreated Di, but that could also be associated with the glucocorticoid treatment. My main concern is the poor appetite... if the tumor has been destroyed, then CNS infiltration of tumor should have not be the cause. You need to talk to your internist and radiation oncologist about these issues.
ReplyDelete